January 21, 2011
Rep. Gabrielle Giffords is now in a rehab facility. We asked a neurosurgeon, Brian Kopell, assistant professor of neurosurgery at the Medical College of Wisconsin and practices at Froedtert Hospital, some questions about the reconstruction of her calvaria and her prognosis. 
Q1: What have you gleaned from news reports that indicate Rep. Giffords is doing well in terms of higher function?
The main indicator that her recovery has been going well is the rapidity of her improvement. Her transfer to a rehabilitation facility today indicates that she has achieved a level of motor and cognitive function that is at minimum interactive with her environment. The reports that she has been tracking her visitors with her vision also indicates a significant level of awareness. Most interestingly, she has been reported to have been playing with an iPad, certainly demonstrating complex cognitive and motor skills.
That being said, it is a bit curious given the rapidity of her improvement that she underwent tracheostomy. Generally speaking, this is a procedure done either due to a) significant upper airway/facial injury or b) severe mental status depression where the patient cannot protect their airway. There has been nothing in the media reports to support either of these scenarios. Furthermore, there has been no explicit media reports of her writing notes to communicate. Certainly if she is able to “play” with an iPad she could write simple notes indicating that her language networks are still relatively intact.
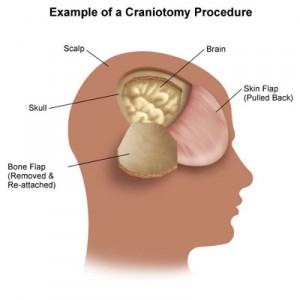
Q2: What does her skull look like now? How do they protect the brain?
Based on media reports, Giffords underwent a decompressive craniectomy during her initial operative management of her GSW. This is a procedure where the surgeons leave the bone flap out to be replaced at a later date should the patient survive the injury. 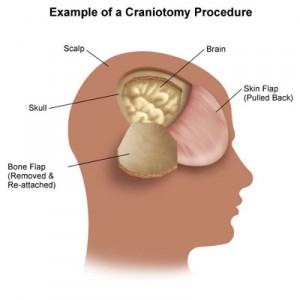 This is done, quite simply, to allow for brain swelling. GSW’s, especially high velocity GSW’s, typically damage the brain in 2 steps. The initial damage occurs due to the trajectory of the bullet through the brain. The deceleration of the bullet in the brain causes a pressure wave that damages surrounding brain tissue. As this damaged brain tissue reacts to this wave, a second stage of damage and swelling commences. It is often this stage that proves fatal for the patient. By leaving out the bone flap, the damaged brain can swell without obstruction and consequent loss of blood flow.
This is done, quite simply, to allow for brain swelling. GSW’s, especially high velocity GSW’s, typically damage the brain in 2 steps. The initial damage occurs due to the trajectory of the bullet through the brain. The deceleration of the bullet in the brain causes a pressure wave that damages surrounding brain tissue. As this damaged brain tissue reacts to this wave, a second stage of damage and swelling commences. It is often this stage that proves fatal for the patient. By leaving out the bone flap, the damaged brain can swell without obstruction and consequent loss of blood flow.
Her head looks quite distorted right now; it is probably why the media will not see Ms. Giffords for a while. Generally, patients with cranial defects are given helmets to wear in order to protect the essentially un protected brain.
Q3: Where now is the section of the calvaria that was removed When/how will they replace it?
Typically, surgeons do one of two things with the bone flap. Some make a subcutaneous pouch in the abdomen an place it there. It is a sterile environment. Others place it in a sterile refrigeration unit in the hospital specially designed to house such specimens.
We typically replace the bone flap 2-6 months after injury depending on circumstance and patient recovery. It is a simple procedure in which the old scalp incision is reopened and the bone flap is affixed over the defect with a variety of fixation methods (I use small titanium plates). Depending on the time elapsed, there can be some significant remodeling of the calvarial defect that requires some drilling of the bone flap in order to make a good cosmetic result.
Should an infection develop, the old bone flap would need to be removed. In this case, a high-resolution CT can be obtained and a 3D reconstruction of the defect can be modeled. This information can be used to develop a custom acrylic implant with CAD modeling techniques.